
Credentialing for New Healthcare Providers: Overcome Common Challenges
Table of Contents
- Introduction: The Importance of Credentialing for New Healthcare Providers
- Common Credentialing Mistakes and How to Avoid Them
- Streamlining the Credentialing Process for Faster Enrollment
- Navigating Payer Networks: Key Considerations for New Providers
- Overcoming Specific Challenges for New Providers
- Conclusion: Ensuring Credentialing Success for New Providers
Starting out as a new healthcare provider is an exciting step in your career. You’re ready to make a difference, serve patients, and build a thriving practice. But before you can begin, there’s one crucial hurdle to clear: credentialing. This process ensures that you meet all qualifications, licenses, and payer requirements to treat insured patients and receive reimbursements.
While credentialing is essential, it can feel overwhelming for new providers. Between managing piles of paperwork, keeping up with payer-specific rules, and navigating long timelines, it’s easy to feel stuck. Mistakes or delays can stall your start, disrupt your cash flow, and leave you frustrated.
The good news? With a strategic approach, you can simplify the credentialing process, avoid common pitfalls, and get enrolled in payer networks faster. This guide breaks down practical steps to help you navigate credentialing successfully and start your healthcare journey on the right foot.
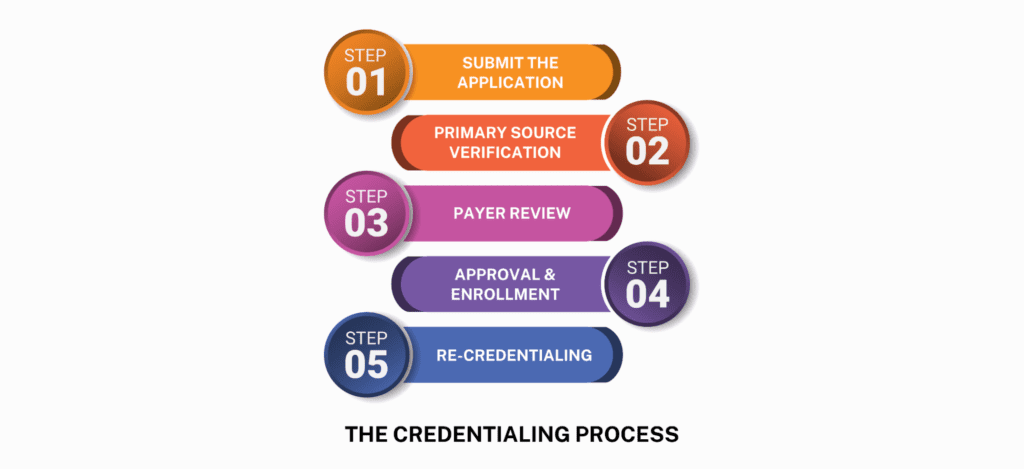
Credentialing is the process of verifying a provider’s professional qualifications, including licenses, certifications, education, and work history. It’s a mandatory step for joining insurance networks, treating insured patients, and ensuring compliance with payer and regulatory standards.
For new providers, credentialing directly impacts your ability to:
- Start Seeing Patients: Without credentialing, you can’t treat insured patients or bill insurance companies.
- Grow Your Practice: Credentialing allows you to join payer networks, making your services accessible to a larger patient base.
- Maintain Financial Stability: Accurate credentialing ensures you get reimbursed for the care you provide.
Given its importance, tackling credentialing efficiently is the first step in launching a successful healthcare career.
For new providers, mistakes during credentialing are common—but they’re also avoidable. Here are some frequent pitfalls and ways to sidestep them:
-
Missing Documentation: Incomplete applications are a leading cause of credentialing delays. Missing a single piece of information, like a license copy or malpractice insurance, can stall the process.
Solution: Create a checklist of all required documents—licenses, certifications, insurance, references, and IDs—and double-check everything before submission. Keep both digital and physical copies for easy access. -
Inaccurate or Outdated Information: Simple errors like an incorrect address, expired certifications, or outdated contact details can lead to rejections.
Solution: Carefully review your application to ensure every detail is current and accurate. Verify licenses and certifications are valid and renew any nearing expiration. -
Delayed Responses to Payer Requests: Payers often ask for additional information or clarification during credentialing. Slow responses can drag out approval timelines.
Solution: Assign yourself (or a trusted team member) the task of monitoring payer communications daily. Prompt responses help keep the process moving forward.
By staying organized, detail-oriented, and proactive, you can avoid these common mistakes and keep the credentialing process on track.
Streamlining the credentialing process is key to getting enrolled faster and with fewer headaches. Here are actionable steps to simplify the journey:
- Organize Your Paperwork: Start by gathering all your credentials—licenses, education certificates, malpractice insurance, and any required references—into a centralized folder. Digital cloud storage tools can help you organize files securely and keep track of expiration dates.
- Leverage Credentialing Software: Credentialing management software automates the tedious parts of the process. It tracks application statuses, sends reminders for renewals, and manages document submissions, reducing human error and saving you time.
- Consider Outsourcing: If you find the process overwhelming, outsourcing to credentialing experts can be a game-changer. Professionals who specialize in credentialing understand payer requirements, handle the paperwork, and follow up on your behalf, ensuring accuracy and faster approval.
- Follow Up Regularly: Submitting your application is just the beginning. Regularly check with payers on the status of your application and address any issues promptly. Proactive follow-ups ensure your application doesn’t fall through the cracks.
Joining the right payer networks is critical to reaching the patients you want to serve. Here’s how to approach it:
-
Understand Payer Requirements: Each insurance network, whether commercial insurers, Medicare, or Medicaid, has its own application process and requirements.
Tip: Research each payer’s guidelines ahead of time and tailor your applications accordingly. - Prioritize Relevant Networks: Focus on the payers that align with your patient demographics and specialty. For example, a pediatrician may prioritize Medicaid participation, while a specialist might target specific commercial insurers.
- Negotiate Contracts Wisely: Once credentialed, review your contracts carefully. Pay attention to reimbursement rates, terms, and conditions. Don’t hesitate to negotiate rates that reflect the value of your services—this can have a major impact on your practice’s financial success.
New providers often face additional hurdles, such as long credentialing timelines, multi-state requirements, and staying compliant over time. Here’s how to tackle them:
- Managing Timelines: Credentialing can take anywhere from 60 to 120 days. Start early—ideally as soon as you secure your position or before your practice opens—to avoid delays.
- Multi-State Credentialing: If you plan to practice in multiple states, each will have its own licensing and credentialing requirements. Credentialing software or outsourced services can help you manage these complexities.
- Staying Compliant: Credentialing isn’t a “set it and forget it” process. Track renewal deadlines for licenses, certifications, and insurance to avoid lapses. Automated reminders can help ensure you stay compliant.
Credentialing is more than an administrative necessity—it’s the foundation of your success as a healthcare provider. It opens the door to treating insured patients, ensures compliance with payer standards, and establishes your practice’s credibility and financial stability. By avoiding common mistakes, leveraging tools and expertise, and staying proactive, you can simplify the credentialing process and set your practice on the right path from day one.
Remember, credentialing isn’t a one-time task but an ongoing commitment to maintaining excellence in your profession. As your practice grows, a solid credentialing foundation will ensure uninterrupted patient care, steady revenue, and lasting trust with payers and patients alike.
At RevGroMD, we’re here to make credentialing seamless, accurate, and stress-free, so you can focus on delivering quality care and achieving your long-term goals. Partner with us today to secure your practice’s future and thrive in your healthcare journey.
