Strategies to Optimize Revenue Cycle Management
Introduction
In the dynamic world of healthcare, financial health is as crucial as providing quality patient care. Revenue Cycle Management (RCM) plays a pivotal role in ensuring that healthcare practices remain financially viable and capable of delivering exceptional services. Successful RCM involves all administrative and clinical functions that impact the ‘capture, management, and collection’ of patient service revenue.
Each step must be executed flawlessly to ensure that healthcare providers are reimbursed in a timely manner and avoid the common pitfalls that lead to revenue leakage.
Below are some best practices and strategies for optimizing RCM, focusing on the critical aspects of patient registration, coding and billing accuracy, claims management, and enhancing cash flow.
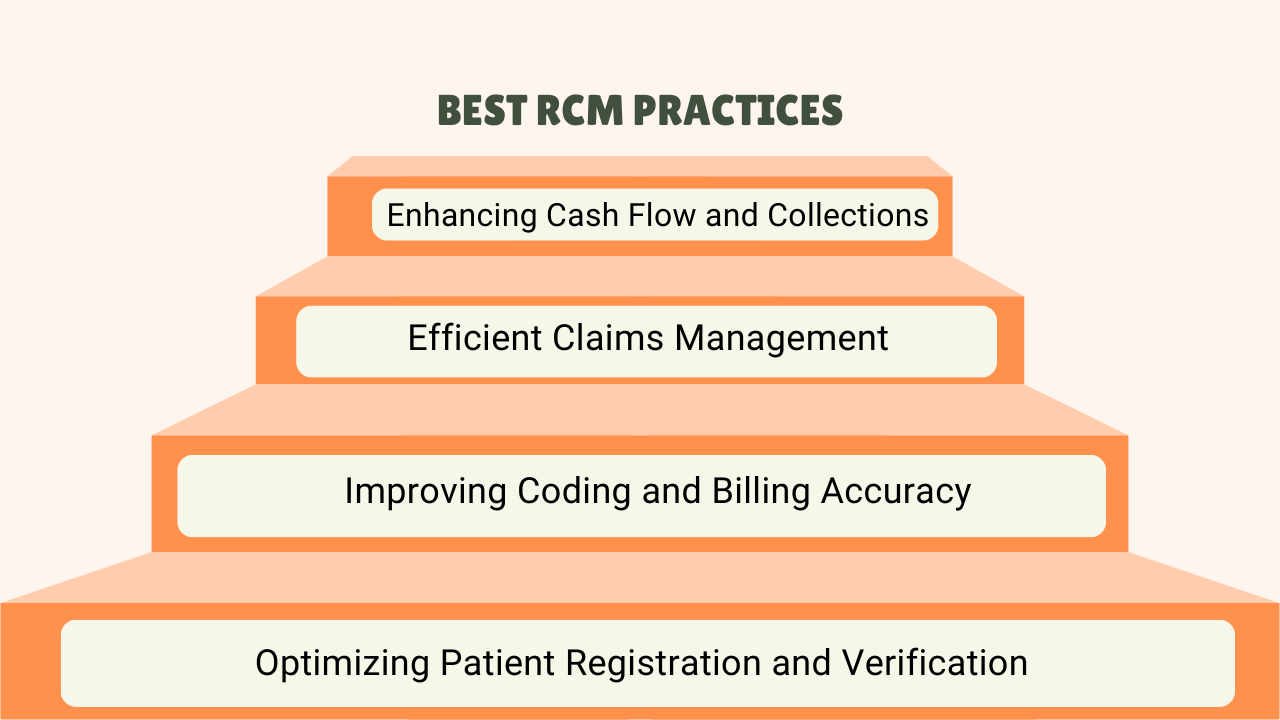
1. Optimizing Patient Registration and Verification:
- Ensuring Right Patient Information
Right patient information is the base of a successful RCM. It will therefore ensure that all patient details are accurately captured in their registration to avoid denial of claims and delays. The verification process should include insurance eligibility, demographic information, and acquisition of required authorizations.
- Preventing Revenue Leakage: Eliminating Registration Errors
A major source of revenue leakage comes from registration errors that result in denied claims and lagging payments. Such errors can be prevented by setting up good verification processes and training the staff to handle patient information with care. Automated systems that double-check information against each other in real time are also important in this regard.
2. Improving Coding and Billing Accuracy:
- The Impact of Coding Accuracy on Reimbursements
Correct medical coding is fundamental in achieving appropriate reimbursements. Wrong coding may lead to claim denials, underpayments, or, at worst, be subjected to investigative review. Proper and accurate coding that aligns with the care being delivered will only ensure optimization of revenue and keep the provider in good payer compliance.
- Solutions for Enhancing Billing Process and Reducing Denials
The coding staff should be trained; there should be regular auditing for coding, and updated billing software should be used. Practices should establish a clear protocol for handling denials, including identifying common denial reasons and implementing corrective actions. Update coding practices periodically as and when required with changes in regulations and payer requirements.
3. Efficient Claims Management
- Importance of Timely and Accurate Claims Submission
Timely and accurate claims submission is the key to a continuous flow of cash. Late claim submissions can miss payment windows and increase the probability of denials. So, practices must have in place a good process for submitting claims that are valid, clean, and complete before they leave the four walls of the practice.
- What are some strategies for resolving Claims Denials and Rejections?
Resolving claims denials and rejections includes identifying the source of them as well as preventing them from happening. Practices should develop a denial management process that supports tracking denials, analyzing trends, and appealing denied claims promptly. In addition, it is always helpful to communicate with the payers on a regular basis, to ensure problem resolution and to gain insight into policy changes.
4. Enhancing Cash Flow and Collections
- Streamlining Payment Processes to Improve Cash Flow
The key to enhancing cash flow is to streamline the payment processes. Streamlining of payment processes may become accelerated by adopting electronic payment systems, multiple payment options, clear payment policies, clear billing statements that are sent out in a timely manner.
- Best Practices for Effective Patient Collections and Follow-Up
Effective patient collections should involve clear communication with patients concerning their payment expectations and policy. Practices must notify patients of their financial obligations with the greatest possible specificity and furnish payment plans in a flexible manner if necessary. Collection rates can also be boosted by automated reminders about balances due and staffers who focus exclusively on collections.
Conclusion
Effective Revenue Cycle Management is crucial for maintaining the financial health and growth of healthcare practices. By improving patient registration and verification, ensuring accurate coding and billing, and streamlining claims management and collections, practices can reduce revenue loss and enhance their reimbursement potential.
Adopting these best practices not only safeguards your practice’s financial performance but also elevates patient satisfaction by providing a more transparent and efficient billing process.
Ready to transform your practice’s financial health? Our expert RCM services are designed to streamline your operations, reduce administrative burdens, and maximize your revenue potential. Don’t let inefficient processes stand in the way of your practice’s success—reach out to us today to discover how RevGroMD’s tailored RCM solutions can give you a competitive edge and secure you practice’s financial future.
